What is Peripheral Arterial Disease (PAD)?
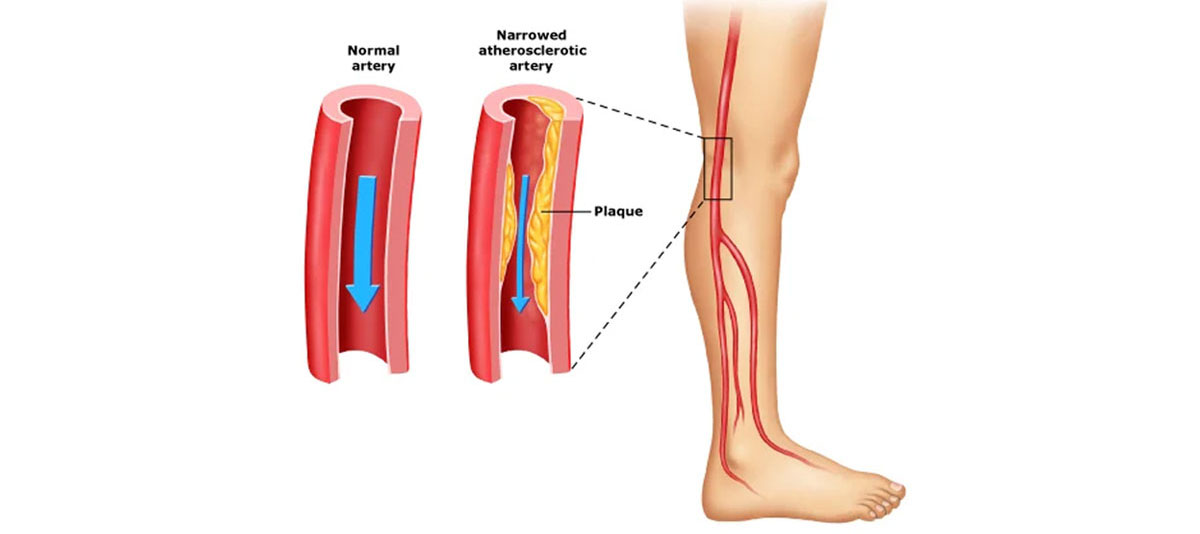
PAD is a circulatory issue. Narrowed arteries restrict blood flow to the limbs. This occurs more commonly in the lower legs. The limbs do not receive enough blood to keep up with the demands of day-to-day use,resulting in pain when walking. The condition can reduce blood flow to the heart and brain.
What causes PVD?
The most common cause of PVD is atherosclerosis, the buildup of plaque inside the artery wall. Plaque reduces the amount of blood flow to the limbs. It also decreases the oxygen and nutrients available to the tissue. Blood clots may form on the artery walls, further decreasing the inner size of the blood vessel and block off major arteries. Other causes of PVD may include:


Risk factors for peripheral vascular disease include:
- Family history of heart disease, high blood pressure, high cholesterol, or stroke
- Older than 50 years
- Overweight or obesity
- Inactive (sedentary) lifestyle
- Smoking
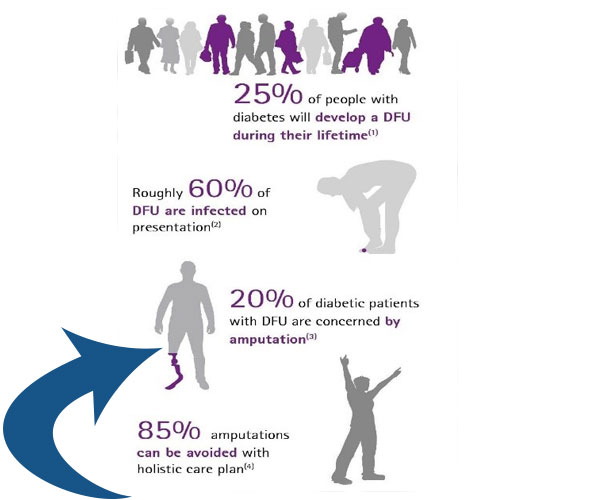
- Diabetes
- High blood pressure
- High cholesterol or LDL (the 'bad cholesterol'), plus high triglycerides and low HDL (the 'good cholesterol')
- Pain in the buttocks, hips, thighs, calves, ankles or feet during walking (a condition called claudication)
- Pain in the leg, calves, ankles, or feet at rest
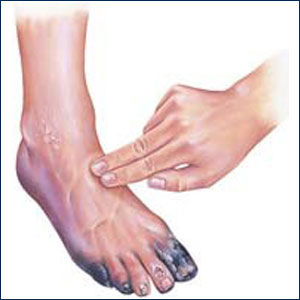
- Ulceration or gangrene involving the legs, most commonly in the foot/toes
- Nerve damage with pain, tingling, or numbness in the lower leg, ankle, and foot
- Weakness in the involved leg
- Coldness in the lower leg and foot
- Weak or absent pulses in the involved leg
- Color changes in the involved leg
- Erectile dysfunction in men
- In severe cases,
If the blood supply is very much reduced then you may develop pain even at rest, particularly at night when the legs are raised in bed. Typically, rest pain first develops in the toes and feet rather than in the calves. Sores (ulcers) may develop on the skin of your feet or lower leg if the blood supply to the skin is poor. In a small number of cases, tissue death (gangrene) of a foot may result. However, this is usually preventable (see below).
The longer you wait, the fewer treatment options will be available. Many PAD treatment options, such as atherectomy, stenting, and angioplasty, are minimally invasive procedures that can often restore full mobility within a week of treatment. However, these treatment options may not be an option in advanced stages of PAD, when the blockage hardens, is spread over large areas, or is in areas too difficult to access. Severe PAD may require bypass graft surgery, which is an invasive surgical procedure with a longer recovery period and more risks. At its latest stages, amputation of the limb with the blocked blood vessel may be the only option to treat PAD. Some people assume that since their doctor isn’t bringing up peripheral artery disease, it must not be an issue. Risk for PAD increases with age, but can still be found in middle-aged adults. In fact, 1 in 20 adults over the age of 50 have PAD.
If you are a smoker, diabetic, or possess any other risk factor for PAD, your chances of experiencing PAD at a younger age are drastically increased.iv PAD symptoms will worsen over time without medical and/or lifestyle interventions. PAD is caused by a buildup of plaque within the arteries. The first symptom of PAD is usually pain after walking for a moderate distance, which resolves after a short period of rest. Because the pain resolves itself, patients with PAD will frequently adopt a more sedentary lifestyle, to avoid the discomfort of physical activity. However, over time, the buildup of plaque will worsen, restricting blood supply further until there is discomfort walking shorter and shorter distances, and eventually, many people even experience pain at rest. The longer you wait, the more expensive, invasive, and inconvenient the treatment will get. In addition to the increased invasiveness and risks associated with bypass graft surgery in the leg and limb amputation, advanced stage PAD treatments also have longer recovery times, extensive hospital stays, and require physical therapy to return to an independent lifestyle. When compared to a minimally invasive treatment like an angioplasty, there is far less expense, and patients can many times return to work and their normal activities in as little as two days.vi PAD can lead to gangrene. Peripheral artery disease occurs as a result of blockage of the blood vessels that supply blood to the lower extremities. This blood carries valuable oxygen to nourish the tissues and keep them healthy. When that blood supply is depleted, tissue decomposes, and can result in gangrene. This gangrenous tissue can be both limb- and life-threatening, and should be treated immediately.PAD can lead to amputation.
Along with a complete medical history and physical exam, other tests may include:
- Ankle-brachial index (ABI). An ABI is a comparison of the blood pressure in the ankle with the blood pressure in the arm using a regular blood pressure cuff and a Doppler ultrasound device. To determine the ABI, the systolic blood pressure (the top number of the blood pressure measurement) of the ankle is divided by the systolic blood pressure of the arm.
- Doppler ultrasound flow studies. This uses high-frequency sound waves and a computer to create images of blood vessels, tissues, and organs. Your doctor may use the Doppler technique to measure and assess the flow of blood. Faintness or absence of sound may mean blood flow is blocked.
- Magnetic resonance angiography (MRA). This noninvasive test uses a combination of a large magnet, radio frequencies, and a computer to produce detailed images of organs and structures in the body. Your doctor injects a special dye during the procedure so that blood vessels are more visible.
- Computerized tomography angiography (CTA). A CTA imaging test shows the doctor an image of the blood vessels, including areas that have narrowed or become blocked.
- Angiogram. This is an X-ray of the arteries and veins to detect blockage or narrowing. This procedure involves inserting a thin, flexible tube into an artery in the leg and injecting a contrast dye. The contrast dye makes the arteries and veins visible on the X-ray.
The above are primarily used to diagnose PVDs. Ankle-Brachial Index is very inexpensive test and should be adopted earlier before getting other tests done. - Coldness in the lower leg and foot
- Weak or absent pulses in the involved leg
- Color changes in the involved leg
- Erectile dysfunction in men
- In severe cases,
If the blood supply is very much reduced then you may develop pain even at rest, particularly at night when the legs are raised in bed. Typically, rest pain first develops in the toes and feet rather than in the calves. Sores (ulcers) may develop on the skin of your feet or lower leg if the blood supply to the skin is poor. In a small number of cases, tissue death (gangrene) of a foot may result. However, this is usually preventable (see below).
A major problem with PVD/PAD is that almost 50% of patient do not show symptoms. In cases where the patients do show symptoms, many a times it is brushed aside as the symptoms appear generic and an expert doctor is not consulted in time. A delayed diagnosis and delay in treatment can result into extreme complications. If you are experiencing any problem as mentioned in symptoms section above immediately consult an interventional radiologist as they are best trained to treat PVDs. If you do not have any symptoms as but have any heart disease, cholesterol, blood pressure, diabetes, or any kidney disease you should regularly get yourself checked for PVD. All people above age 50 years are also highly recommended for evaluation on regular basis.
- Medicines A medicine called clopidogrel is usually advised. This does not help with symptoms of PAD but helps to prevent blood clots (thromboses) forming in blood vessels (arteries). It does this by reducing the stickiness of platelets in the bloodstream. If you cannot take clopidogrel then alternative antiplatelet medicines such as low-dose aspirin may be advised.
A statin medicine is usually advised to lower your cholesterol level. This helps to prevent a build-up of fatty patches (atheroma).
If you have diabetes then good control of your blood sugar (glucose) level will help to prevent PAD from worsening.
If you have high blood pressure (hypertension) then you will normally be advised to take medication to lower it.
Other medicines are sometimes used to try to open up the arteries - for example, cilostazol and naftidrofuryl. One may be given and may help. However, they do not work in all cases. Therefore, there is no point in continuing with these medicines if you do not notice an improvement in symptoms within a few weeks. - Endovascular Treatment
The treatment of PAD can reduce your symptoms, improve your quality of life, reduce your risk of a heart attack or stroke, and prevent worsening conditions. Left untreated, PAD can worsen and often become life-threatening.
Our treatment goal is to restore blood flow to your limbs by minimizing the narrowing of the arteries. We offer minimally-invasive treatment options called: - Angioplasty
- Stent Placement
- Atherectomy
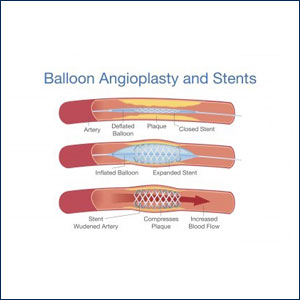
- ANGIOPLASTY:
Angioplasty is a minimally invasive procedure that opens narrowed or blocked blood vessels supplying blood to your legs. A balloon-tipped catheter (a thin hollow tube) will be inserted into a blood vessel in your upper thigh area (called the groin). This is often referred to as a “pin-hole incision.” The catheter is positioned in the narrowed or blocked artery by using a continuous x-ray guidance.When the catheter is in place, the balloon inflates for short amount of time. The plaque is compressed outward against the artery wall, widening the artery and restoring the blood flow. Next, the balloon is deflated and the catheter is removed from your body - STENT PLACEMENT:
Stents are commonly implanted during the balloon angioplasty procedure. A stent is a flexible, metal, mesh tube that expands to hold open the impacted artery. Stents provide internal structural support to better maintain proper circulation and will remain in the previously blocked vessel.Local anesthesia or moderated sedation is administered at the beginning of the procedure to provide enough sedation to make the procedure as comfortable as possible. You will be awake the entire time! - ATHERECTOMY:
Artherectomy uses a catheter and x-ray guidance, similar to the angioplasty and stent placement. Instead of inserting a balloon, however, the atherectomy catheter has a sharp blade at its end designed to remove and collect plaque from your blood vessel. The catheter is taken out of the vessel once sufficient plaque is removed.
We have very fast and competent working team which provide you comfortable atmosphere and ease your nerves. Usual time of stay is around 2-3 Days.
You can resume your work after 2-3 days if existing disease allows