Interventional radiology has become an integral part of patient care services offered at many secondary and tertiary care hospitals in India. In addition to the routine elective consultation and procedural care for various vascular, nonvascular, and oncologic conditions, the interventional radiology service is being increasingly involved in the treatment of emergency conditions such as acute stroke or acute pulmonary embolism, deep venous thrombosis, Acute arterial thrombosis, Acute Bleeder managements. The emergency interventional radiology service is more challenging compared with the elective service in several aspects, including, but not limited to, the need for quick decision-making given the clinical status of the patient, availability of resources for early intervention, and availability of alternative therapeutic options. As interventional radiologists, we are committed to providing emergency interventional services. It is important that we, as a society, work together with the hospitals in laying guidelines for emergency interventional radiology service. This would not only improve the patient care and visibility of interventional radiology as one of the pillars of medicine but also enhance the appeal of interventional radiology as a specialty for future medical graduates
Deep Vein Thrombosis
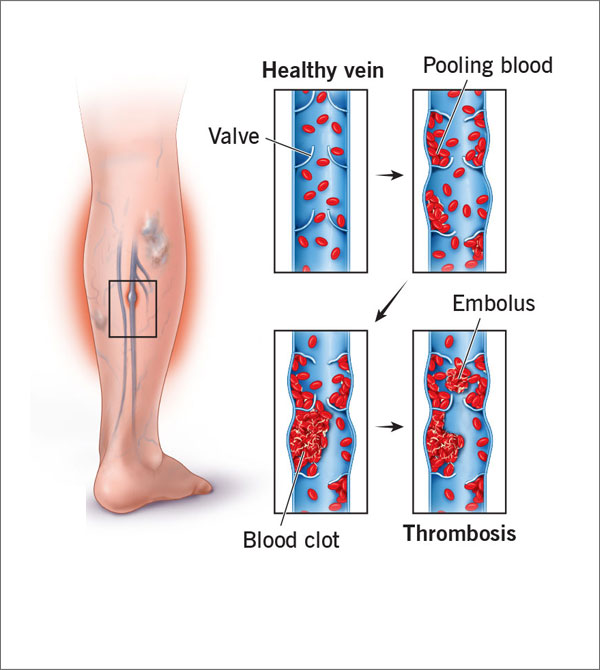
Veins are the blood vessels that transport blood from various body parts to the heart.
A serious medical condition in which a blood clot is formed in a vein deeply inside body is called Deep vein thrombosis (DVT). A blood clot that mostly is in a jelly like state is formed in the veins. It is normally observed that DVT occurs in the thigh or lower leg area, however Deep Vein Thrombosis can happen in any other areas of human body.
Sometimes condition of Deep Vein Thrombosis is also sometimes referred as Post Thrombotic Syndrome, Post Phlebitic Syndrome & Thromboembolism though the former two are conditions which are outcome of prolonged existence of DVT.
Sometimes the clot so identified as DVT breaks free, and flow to other vital organs in the body. Incidence wherein clots are observed to block flow to lungs is called pulmonary embolism and is considered life threatening.
There is no single factor identified to be the cause of DVT. DVT as condition is observed to be developed due to various factors or combination thereof. Some of the factors which are known to be the cause of DVT or which increase the probability of a person developing Deep vein Thrombosis are listed below:
- Heredity: It is observed that people with a family history of Deep Vein Thrombosis have significant high chances of developing DVT themselves.
- Weight: People who are overweight or obese tend to develop DVT as more pressure is exerted on veins in legs and pelvis.
- Any injury resulting in damage to veins may lead to onset of clot formation in the deep veins i.e. DVT as any major injury may affect the inner lining of any deep vein leading to clots.
- Medical conditions/ illnesses like heart disease, lung diseases, bowel inflammation disease, cancer also highly risk the chance of clot formations in veins.
- Pregnancy/ Hormonal therapy/ Consumption of birth control pills: All these may lead to increase in level of “Estrogen” in female body and which may assist in easy clot formation.
- Long Bed Rest or Seated for a long time: Non-movement of muscles for a longer duration sometimes lead to pooling of blood in lower legs and if combined with any other factors mentioned it greatly assists in development of Deep vein Thrombosis.
While development of DVT is more probable with increase in age, existence of any of the above factors may lead to onset of Deep vein Thrombosis at younger age.
DVT is difficult medical condition to identify as many patients (50%) may not display any symptoms. Also, the symptoms are more generic and are shared among various medical conditions. Patients may not be aware of DVT till they experience a serious life-threatening medical incidence like pulmonary embolism. Some of the common symptoms are:
- Leg or foot swelling (sometimes only in one leg)
- Pain, cramp or tenderness in the leg (usually in calf region)
- Warmer skin that feels warmer than the surrounding skin
- Reddish or Discoloured skin over the pain area
While the above symptoms may appear generic and one may not feel the need of medical evaluation, it is to be remembered that DVT leads to lethal incidences like Pulmonary Embolism hence shouldn’t be ignored.Patients experiencing above symptoms are advised for medical treatment, below are listed some symptoms which a patient having life-threatening incidence of Pulmonary Embolism may experience and hence should be immediately evaluated by qualified medical professionals.
- Shortness of Breath
- Rapid Breathing with Chest Pain
- Light headedness
- Rapid Heartbeat
- Excessive Sweating
- Coughing with bloody sputum
Primary evaluation of DVT is done by conducting a physical evaluation by medical professional. Clinical confirmation of DVT is done by performing some of the below mentioned tests as required by the medical doctor.
- Ultrasound:With the help of medical device, sound waves are used to identify the existence and development of blood clots.Many a times a series of ultrasounds are required over period to determine growth and development blood clots. This is the most preferable primary test for DVT.
- Venography: Under this X-Ray is taken of dye induced veins to identify the clot formation.
- MRI/ CT:These tests provide visual images of veins and reveal if any clot formation has happened.
- Blood test: While the above radiology tests confirms presence of clots, blood tests are done to obtain corroborative confirmations for DVT like higher levels of a substance called D dimer.
- Medication – Anti Coagulants (Blood Thinners):
Primary treatment and the only non-interventional treatment option for patients, under this method patients are given medications which prevent any future clot formation and hence prevent any spread of DVT.
Though primary treatment, it should be noted that this may not be best suitable for existing clots and your doctor may suggest following interventional procedures to reduce risks and prevent any incidence. - CatheterDirected Thrombolysis (Clot Busting):
Catheter Directed Thrombolysis(CDT) is the most preferred and effective treatment option for existing blood clots. It is usually recommended when patient is identified with multiple grown clots at the time of diagnosis or the doctor needs to ensure prevention of any untoward incidence which may not be avoided with medications.
Catheter Directed Thrombolysis(CDT) is the most preferred and effective treatment option for existing blood clots. It is usually recommended when patient is identified with multiple grown clots at the time of diagnosis or the doctor needs to ensure prevention of any untoward incidence which may not be avoided with medications. - Percutaneous Mechanical Thrombectomy:Percutaneous mechanical thrombectomy(PMT) offers the benefit of early thrombus removal, while limiting thrombolytic dosages and bleeding complications. PMT additionally offers a treatment option for patients with absolute contraindications for lytic therapy as the AngioJet (Medrad, Inc., Warrendale, Pennsylvania), a PMT device discussed below, is the only device that can be used without the addition of lytics. PMT has further been shown to be more cost-effective than alternative treatment regimens when considering the lower thrombolytic dosages administered, the decreased length of ICU stay compared to CDT and the decreased long-term morbidity from post-thrombotic syndrome compared to traditional anticoagulation.
- AngioJet Rheolytic Thrombectomy System — Pulse Power Spray Technique:-
The AngioJet catheter system is comprised of a single-use catheter, a single-use pump set and a drive unit. The catheter, which is available in working lengths of 60, 100 and 120 cm, contains a central lumen for infusate and a larger lumen encompassing the central channel, the guidewire and aspirate from the thrombus. The drive unit generates 10,000 psi of pulsatile infusion flow, which is released from the catheter in retrograde-directed high-velocity saline jets. These jets create a localized low-pressure zone (Bernoulli’s principle) at the catheter tip, macerating thrombus and redirecting flow and debris into outflow channels directed behind the catheter tip for aspiration and removal. Access for the AngioJet system requires a 6 Fr introducer sheath. The AngioJet catheter is then advanced over a 0.035 inch guidewire through the thrombus load. While this system was originally intended for use without adjunctive thrombolytics, it has been demonstrated that the addition of lytics to the infusion solution results in decreased treatment time and improved results. We recommend that thrombolytics be routinely used except when contraindicated, as is our practice. While thrombolytic choice and dose will vary dependent upon surgeon preference, we have experienced good results using 10 mg/ 20 mg of Alteplase in 50 ml of sodium chloride infusing solution. With the aspiration port clamped, infusate is released into the thrombosed venous segment during a slow pullback of the catheter, effectively lacing the clot with thrombolytic drug. After 10 minutes the aspiration function of the catheter is turned on. The catheter is then advanced through the thrombosed segment a second time, removing macerated thrombus through the aspiration ports as the catheter is advanced. This process may be repeated if there is remaining thrombus burden at the end of the first pass. Alternatively, as is often our preference, the patient may then undergo catheter-directed thrombolysis in the ICU overnight and return to the operating room the following day for re-evaluation with venography and possible repeat thrombectomy or venous stenting if indicated. Success in thrombus removal, restoration of venous patency and preservation of valvular function have been demonstrated with the use of the AngioJet pulse-power spray technique. - Complications:-
Patient shall experience Haemoglobinuria for 24-48 hrs which is treatable.Isolated case reports of pancreatitis resulting from massive hemolysis with use of the AngioJet system have been reported but appear to be rare occurrences - Filters:
This treatment option is adopted generally when due to certain medical condition Catheter Directed Thrombolysis can not be done for the patient. Specifically designed to prevent incidences like Pulmonary Embolism, under this procedure a device is inserted into the main vein (Vena cava) which takes back blood from lower body to heart.
This device filters blood clots and stops them from moving to parts of your body where they can become dangerous.
Post-thrombectomy evaluation of the venous segment may reveal areas of venous compression, stenosis or recalcitrant thrombus in some of the patients. May-Thurner anatomy is the most common anatomic variant found on completion imaging during the treatment of proximal DVT . This syndrome is characterized by compression of the left common iliac vein by the right common iliac artery against the fifth lumbar vertebra, resulting in venous compression, development of venous scar tissue and eventually venous stenosis. This condition then predisposes the patient to left iliofemoral DVT. With anticoagulation alone, untreated iliac vein obstruction prevents vessel recanalization in 70–80% of patients and clot propagation may continue in up to 40% of cases. Further, patients with iliofemoral DVT and untreated May-Thurner anatomy experience an increased risk of recurrent DVT and universally experience symptoms of post-thrombotic syndrome during follow-up. Adequate treatment of anatomic compression, stenosis or persistent small thrombus after CDT or PMT requires angioplasty and stenting.
While nothing much can be done to change the heredity, risk of developing Deep Vein Thrombosis can be greatly reduced by adopting a healthy and active lifestyle.
- Regular exercise
- No Smoking
- Keeping optimum weight and BMI under check
- Moving feet around at regular intervals during long travels and avoiding long sittings
- Adhering to medications as prescribed by doctor
- Keeping blood pressure and control
- Keeping doctor informed of any DVT issue in the family
- Compression stockings are recommended to prevent swelling and reduce chances of developing clots.
The above if adopted can significantly reduce the onset of Deep Vein Thrombosis.
Patients are anticoagulated post procedure with unfractionated heparin or low-molecular-weight heparin and transitioned to oral warfarin/ Newer anticoagulatns for 6 months (goal international normalized ratio 2.0–3.0). Patients with recurrent DVT or hypercoagulable disorders may require a longer duration of anticoagulation and consultation with primary care physicians is recommended. Patients with venous stents require lifelong aspirin therapy. Follow-up with duplex ultrasonography is also recommended at 1- and 6-month intervals and yearly thereafter.
We have very fast and competent working team which provide you comfortable atmosphere and ease your nerves. Usual time of stay is around 2-3 Days.
Resume to work?
You can resume your work very next day of the procedure preferably in 2- 3 days.