In addition, interventional radiologists manage several nonvascular pathologies including fallopian tube recanalization, drainage of pelvic abscesses and fluid collections, and image-guided biopsy of ovarian or adnexal lesions. We offer women access to a special place created specifically for them, where you can obtain highly specialized interventional services using state-of-the-art equipment in a compassionate, caring environment.

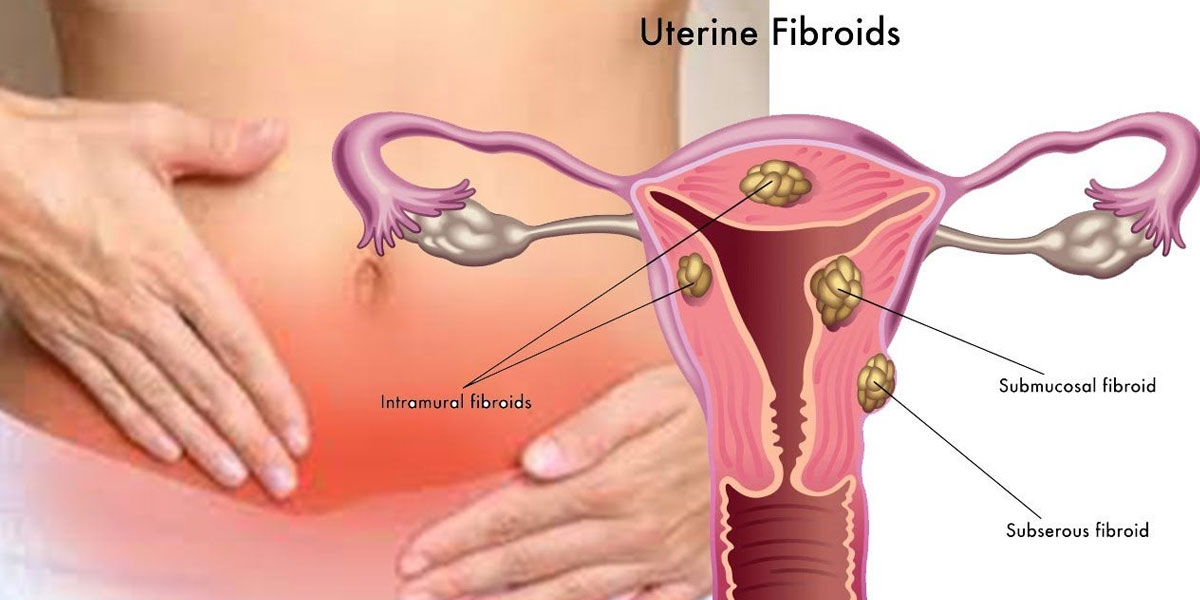
Uterine Fibroid Embolisation
UFE is a non surgical way of treating fibroids by blocking off the arteries that feed the fibroids, the uterine arteries, and making the fibroids shrink. It is performed by an interventional radiologist, rather than a surgeon, and is an alternative to an operation. UFE was first performed in 1995, and since then over 200,000 women have had the procedure performed, world-wide. As with all relatively new procedures, a careful data collection and audit will be performed.
Other tests that you have had done will have shown that you are suffering from fibroids, and that these are causing you considerable symptoms. Your gynaecologist and your GP should have told you all about the problems with fibroids, and discussed with you ways of dealing with them. Previously, most fibroids have been treated by an operation, generally a hysterectomy, where the womb is removed altogether. In your case, it has been decided that embolisation is the best treatment.
A specially trained doctor called an Interventional Radiologist. Interventional radiologists have special expertise in using X-ray equipment, and also in interpreting the images produced. They need to look at these images while carrying out the procedure. Consequently, interventional radiologists are the best trained people to insert needles and fine catheters into blood vessels, through the skin, and place them correctly.
You will lie on the X-ray table, generally flat on your back. You need to have a needle put into a vein in your arm, so that the radiologist can give you a sedative and painkillers. Once in place, this will not cause any pain. You may also have a monitoring device attached to your chest and finger, and may be given oxygen through small tubes in your nose. The interventional radiologist will keep everything as sterile as possible, and will wear a theatre gown and operating gloves. The skin near the point of insertion, probably the groin, will be swabbed with antiseptic, and then most of the rest of your body covered with a theatre towel.
The skin and deeper tissues over the artery in the groin will be anaesthetised with local anaesthetic, and then a needle will be inserted into this artery. Once the interventional radiologist is satisfied that this is correctly positioned, a guide wire is placed through the needle, and into this artery. Then the needle is withdrawn allowing a fine, plastic tube, called a catheter, to be placed over the wire and into this artery.
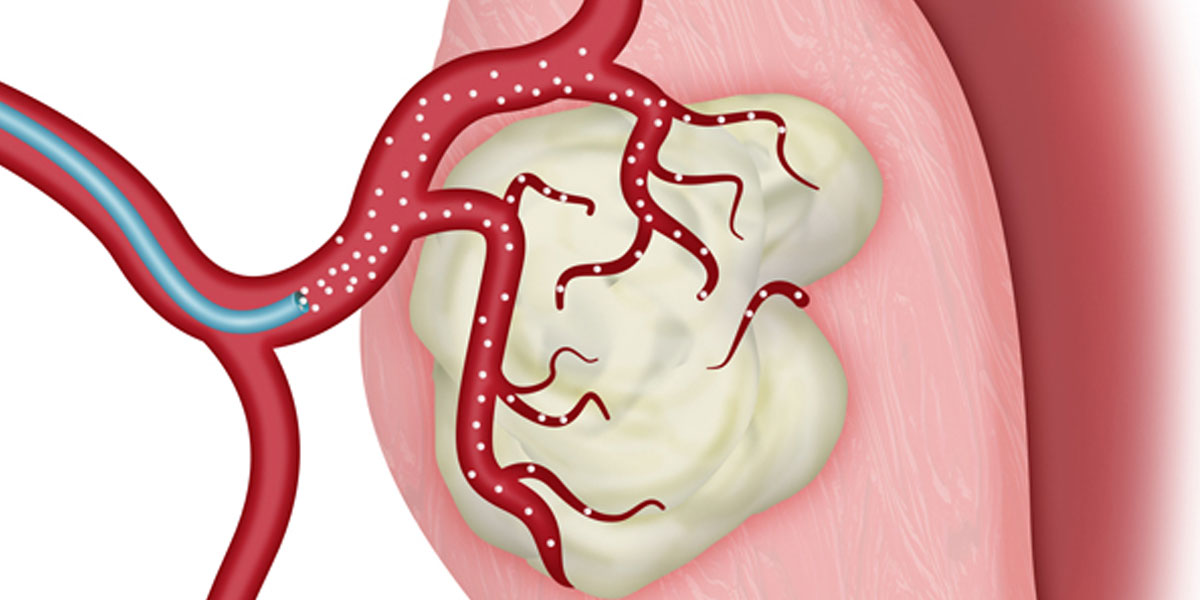
The interventional radiologist will use the X-ray equipment to make sure that the catheter and the wire are then moved into the correct position, into the other arteries which are feeding the fibroid. These arteries are called the right and left uterine arteries. A special X-ray dye, called contrast medium, is injected down the catheter into these uterine arteries, and this may give you a hot feeling in the pelvis. Once the fibroid blood supply has been identified, fluid containing thousands of tiny particles is injected through the catheter into these small arteries which nourish the fibroid. This silts up these small blood vessels and blocks them so that the fibroid is starved of its blood supply
Both the right and the left uterine arteries need to be blocked in this way. It can often all be done from the right groin, but sometimes it may be difficult to block the branches of the right uterine artery from the right groin, and so a needle and catheter needs to be inserted into the left groin as well. At the end of the procedure, the catheter is withdrawn and the Interventional Radiologist then presses firmly on the skin entry point for several minutes, to prevent any bleeding.
When the local anaesthetic is injected, it will sting to start with, but this soon passes, and the skin and deeper tissues should then feel numb. The procedure itself may become painful. However, there will be a nurse, or another member of staff, standing next to you and looking after you. If the procedure does become too painful for you, then they will be able to arrange for you to have some painkillers through the needle in your arm.
As the dye, or contrast medium, passes around your body, you may get a warm feeling, which some people can find a little unpleasant. However, this soon passes and should not concern you.
Every patient’s situation is different, and it is not always easy to predict how complex or how straightforward the procedure will be. Some uterine fibroid embolisations do not take very long, perhaps half an hour. Other embolisations may be more involved, and take rather longer, perhaps an hour. As a guide, expect to be in the X-ray department for about two hours.
Uterine fibroid embolisation is a safe procedure, but there are some risks and complications that can arise, as with any medical treatment.
There may occasionally be a small bruise, called a haematoma, around the site where the needle has been inserted, and this is quite normal. If this becomes a large bruise, then there is the risk of it getting infected, and this would then require treatment with antibiotics.
Most patients feel some pain afterwards. This ranges from very mild pain to severe cramp, period-like pain. It is generally worst in the first 12 hours, but will probably still be present when you go home. While you are in hospital this can be controlled by powerful pain kill/ers. You will be given further tablets to take home with you.
Most patients get a slight fever after the procedure. This is a good sign as it means that the fibroid is breaking down. The pain killers you will be given will help control this fever.
A few patients get a vaginal discharge afterwards, which may be bloody. This is usually due to the fibroid breaking down. Usually, the discharge persists for approximately two weeks from when it starts, although occasionally it can persist intermittently for several months. This not in itself a medical problem, although you may need to wear sanitary protection. If the discharge becomes offensive and if it is associated with a high fever and feeling unwell, there is the possibility of infection and you should contact your interventional radiologist to see your gynaecologist urgently.
The most serious complication of uterine fibroid embolisation is infection. This happens to perhaps two in every hundred women having the procedure. The signs that the uterus is infected after embolisation include great pain, pelvic tenderness and a high temperature.
There are now many good, long term studies of the results of uterine fiberoid embolisation. Over 90% of women will be relieved of their symptoms after UFE and reduction in uterine and fibroid volumes of over 60% are expected. Incomplete death of the fibroids can lead to failure of the treatment in 5-10% of cases and reoccurance of fibroid symptoms can occur in up to 25%. Improvements in equipment and techniques have been made to try to reduce these early failures and late recurrences.
Some women, who could not become pregnant before the procedure because of their fibroids, have become pregnant afterwards. However, if having a baby in the future is very important to you, you need to discuss this with your doctor as it may be that an operation is still the better choice.
Some of your questions should have been answered by this information, but remember that this is only a starting point for discussion about your treatment with the doctors looking after you. Do satisfy yourself that you have received enough information about the procedure, before you sign the consent form.
UFE is considered a safe procedure, designed to improve your medical condition and save you having a larger operation. There are some risks and complications involved, and because there is the possibility of a hysterectomy being necessary, you do need to make certain that you have discussed all the options available with your doctors.
We have very fast and competent working team which provide you comfortable atmosphere and ease your nerves. Usual time of stay is around 2-3 Days.
Resume to work?
You can resume your work very next day of the procedure preferably in 2- 3 days.